Automation of Treatment Planning Processes

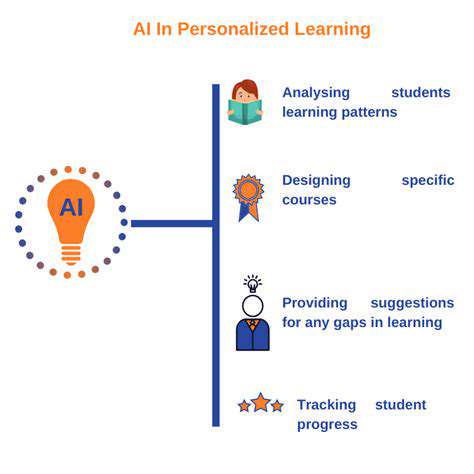
Automated treatment planning systems are revolutionizing the field of healthcare by streamlining and optimizing the process of developing individualized treatment plans. These systems leverage sophisticated algorithms and vast datasets to analyze patient-specific information, such as medical history, imaging scans, and clinical characteristics, to generate comprehensive and personalized treatment recommendations.
The potential benefits of automation in treatment planning are substantial, including improved efficiency and reduced turnaround times. Furthermore, these systems can help minimize human error and ensure consistent quality of care across various healthcare settings.
One key aspect of automated treatment planning is the ability to rapidly process large volumes of data. Traditional methods often rely on manual analysis, which can be time-consuming and prone to errors, particularly when dealing with complex cases or large datasets. Automated systems, on the other hand, can quickly sift through and interpret this data, allowing clinicians to focus on the nuances of each case and make informed decisions.
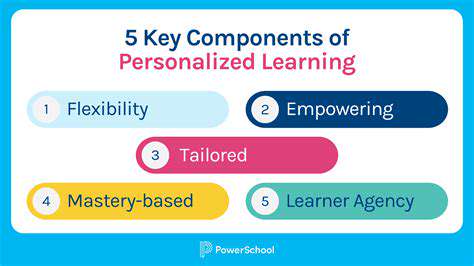
Another significant advantage of automated treatment planning is its capacity for generating personalized treatment options. By considering individual patient characteristics and preferences, these systems can tailor treatment plans to maximize effectiveness and minimize potential side effects. This personalized approach is crucial for ensuring optimal patient outcomes and improving the overall quality of care.
This tailoring of treatment extends to accommodating various patient needs and preferences, leading to enhanced patient satisfaction and engagement in the treatment process.
The integration of automated treatment planning into existing workflows can enhance collaboration among healthcare professionals. This collaborative approach allows for shared access to patient data and treatment plans, facilitating better communication and coordination between clinicians.
Improved communication and streamlined workflows fostered by automation can lead to a more efficient and effective healthcare delivery system. This can ultimately translate into better patient outcomes and a more positive experience for all involved.
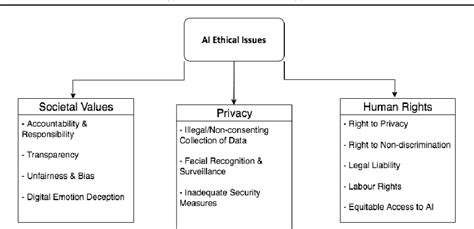
Despite the numerous advantages, the implementation of automated treatment planning systems also requires careful consideration of ethical implications and potential limitations. Maintaining data security and privacy is paramount, and ensuring transparency in the decision-making process is crucial for building trust among patients and healthcare providers.
Furthermore, the development and maintenance of these systems require significant investment in technology and expertise. Addressing these challenges is essential to maximizing the benefits of automated treatment planning and ensuring its responsible and effective implementation.
Challenges and Future Directions of AI in Radiation Therapy
Implementation and Integration Challenges
Integrating AI into existing radiation therapy workflows presents significant challenges. One major hurdle is the need for seamless data integration between different systems and modalities. Current clinical data systems often lack the necessary structure and standardization for AI algorithms to effectively operate. This necessitates substantial investment in data preprocessing and standardization pipelines, which can be time-consuming and costly. Furthermore, the clinical validation and regulatory approval processes for AI-driven tools are complex and lengthy, often delaying the widespread adoption of these technologies in the clinic. This process requires rigorous testing and demonstrating the safety and efficacy of AI systems in a real-world setting, which can be resource-intensive.
Another key challenge lies in the lack of standardized training datasets for AI algorithms. The quality and quantity of available data significantly influence the performance and reliability of AI models. Developing large, diverse, and representative datasets is essential, but this often requires collaboration between multiple institutions and the collection of patient data with explicit consent and ethical considerations. Maintaining the privacy and security of patient data throughout this process is paramount and requires robust data governance and security protocols. The variability in patient characteristics, treatment protocols, and tumor types across different institutions further complicates dataset creation and model generalizability.
Ethical and Societal Implications
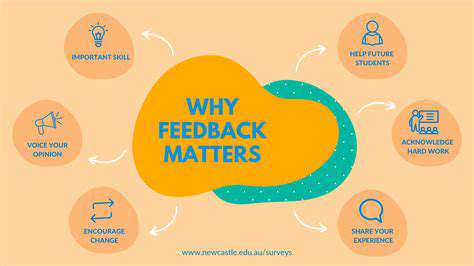
The increasing reliance on AI in radiation therapy raises important ethical considerations. The potential for bias in AI algorithms, stemming from the data they are trained on, needs careful consideration. Algorithms trained on data reflecting existing health disparities could perpetuate or exacerbate inequalities in access to and quality of radiation therapy. Transparent and responsible development and deployment of AI systems are crucial to mitigate these risks and ensure equitable access to cutting-edge treatments for all patients. The need for ongoing monitoring and evaluation of AI algorithms in clinical settings to detect and address potential biases is paramount.
Furthermore, the shift towards AI-driven decision-making in radiation therapy necessitates a thoughtful discussion about the role of human clinicians. The potential for overreliance on AI systems and the loss of essential clinical expertise needs careful consideration. Establishing clear guidelines and protocols for the interplay between human expertise and AI assistance is essential for maintaining the highest standards of patient care. The development of educational programs and training resources for clinicians to effectively utilize AI tools in their practice is also critical.
The potential impact of AI on radiation therapists' roles and responsibilities also warrants attention. How AI might alter the job description and required skill sets for radiation therapists needs further exploration. The need for ongoing professional development and adaptation to the evolving landscape of AI integration into radiation therapy is essential to maintain the workforce's competency and to ensure that AI is used to augment, rather than replace, human expertise.
Finally, the societal implications of AI in radiation therapy extend beyond the clinical setting. The potential for AI to improve treatment outcomes and reduce healthcare costs needs to be carefully weighed against the potential for job displacement and the need for equitable access to AI-powered technologies.