Introduction to AI in Geriatric Care
What is Artificial Intelligence (AI)?
Artificial intelligence, commonly referred to as AI, represents a broad spectrum of technologies designed to replicate human cognitive abilities. These encompass learning from experience, solving complex problems, making informed decisions, and interpreting natural language. By analyzing extensive datasets, AI systems can uncover patterns and insights that often elude human perception. Such capabilities enable automation of routine tasks, boost operational efficiency, and enhance quality of life across various domains.
The field of AI continues to evolve at a rapid pace, with innovative applications emerging regularly. From autonomous vehicles to advanced medical diagnostics, AI is reshaping numerous industries. Its potential to transform healthcare, especially in the realm of elder care, holds particular promise for improving outcomes and quality of life for aging populations.
AI's Potential in Geriatric Care
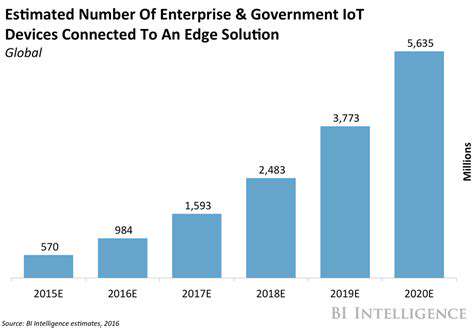
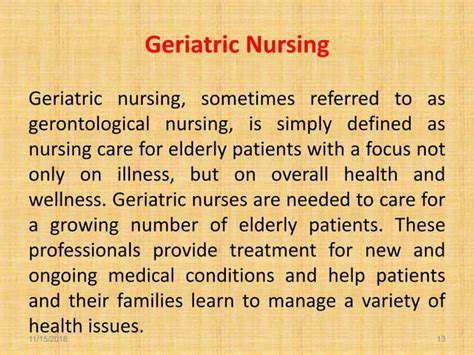
With global populations aging at an unprecedented rate, healthcare systems face significant challenges. AI presents groundbreaking solutions to enhance care for older adults while alleviating pressure on healthcare providers. Through remote patient monitoring, risk prediction, and personalized treatment plans, AI enables more efficient and effective care delivery.
One transformative application involves sophisticated predictive analytics. By examining comprehensive patient data including medical histories, lifestyle factors, and genetic information, these models can identify individuals at risk for specific health conditions. Such proactive approaches facilitate early intervention and preventive measures, ultimately improving health outcomes.
Applications of AI in Daily Geriatric Care
AI-powered tools are increasingly being integrated into routine elder care. These solutions automate administrative tasks like appointment scheduling, medication management, and vital sign tracking, allowing healthcare professionals to dedicate more time to direct patient care.
Diagnostic tools powered by AI represent another significant advancement. These algorithms can detect subtle abnormalities in medical imaging such as X-rays and CT scans, enabling earlier diagnoses and more precise treatment planning.
Ethical Considerations and Future Directions
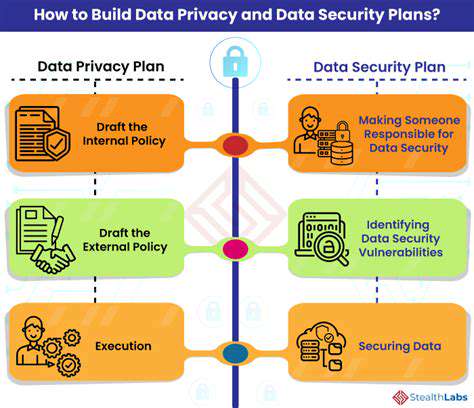
As AI becomes more prevalent in geriatric care, addressing ethical implications becomes paramount. Key concerns include data privacy protection, mitigation of algorithmic bias, and ensuring equitable access to technology. Implementing robust safeguards and regulatory frameworks is essential for responsible use of AI with sensitive patient information.
The future of AI in elder care appears exceptionally promising, with ongoing research paving the way for more innovative solutions. Advances in machine learning, natural language processing, and robotics will enable increasingly sophisticated, personalized approaches to care delivery. These developments stand to significantly improve quality of life for aging populations while ensuring they receive optimal care throughout their later years.
Predictive Modeling for Early Intervention
Predictive Modeling Techniques
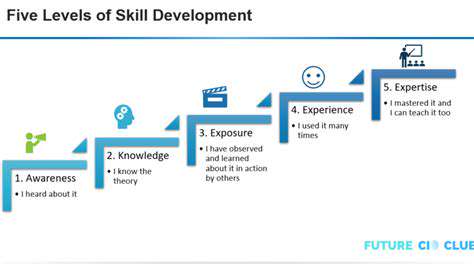
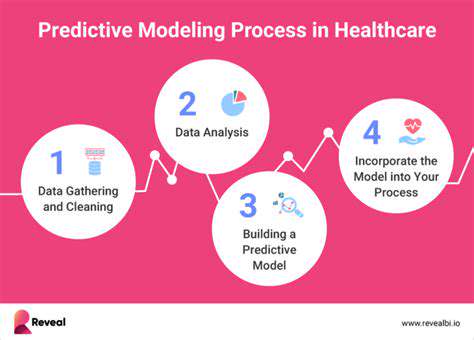
Predictive modeling fundamentally employs statistical algorithms and machine learning methods to anticipate future outcomes using historical data. These analytical models examine patterns and relationships within datasets to identify influential factors, enabling data-driven decision making and proactive planning. The process incorporates various methodologies ranging from basic linear regression to advanced neural networks, each suited to different analytical contexts.
Data Preparation and Feature Engineering
Effective predictive modeling requires meticulous data preparation. This includes data cleansing, handling incomplete records, and transforming variables for optimal model compatibility. Feature engineering, a critical component, involves creating derived variables that enhance model predictive performance. Attention to data quality and feature selection profoundly impacts the accuracy and reliability of resulting predictions.
Model Selection and Training
Selecting appropriate predictive models is crucial for achieving optimal results. Considerations include data characteristics, desired outcomes, and available computational resources. Choosing and properly training the right model significantly influences prediction accuracy and effectiveness.
Model Evaluation and Validation
Assessing model performance is essential for ensuring reliability. Common evaluation metrics include accuracy, precision, recall, and F1-scores. Comprehensive validation using independent datasets prevents overfitting and confirms model generalizability. This process facilitates model refinement and identifies areas for improvement.
Deploying and Monitoring Predictive Models
Following validation, predictive models can be implemented in operational environments. Integration with existing systems enables automated prediction generation. Continuous performance monitoring ensures sustained accuracy and adaptability to changing conditions. This includes detecting data drift or other factors that might compromise prediction quality.
Applications of Predictive Modeling in Early Intervention
Predictive modeling finds diverse applications in early intervention strategies. Healthcare applications include identifying high-risk patients for early preventive measures. Educational implementations can pinpoint students needing academic support, enabling personalized learning plans. Additional applications span business forecasting, environmental monitoring, and other domains where proactive problem-solving proves valuable.
AI-Assisted Exercise and Therapy Monitoring
AI's Role in Enhancing Exercise Adherence
AI-enhanced exercise programs significantly improve compliance in geriatric rehabilitation. By providing personalized feedback and dynamically adjusting routines based on real-time performance data, these programs increase engagement and motivation among older adults. This tailored approach accommodates individual needs and preferences, fostering greater commitment to rehabilitation and ultimately improving outcomes.
Real-Time Monitoring for Precise Feedback
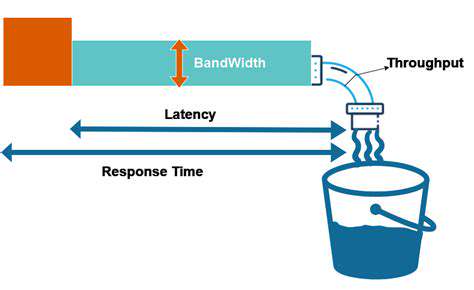
AI algorithms process data from wearable devices in real-time, offering immediate feedback to patients and therapists. This enables continuous adjustment of exercise parameters to ensure optimal progress while identifying potential issues like fatigue or discomfort for timely intervention.
Predictive Analytics for Proactive Interventions
Advanced AI models can forecast potential rehabilitation challenges by analyzing patient data. This predictive capability allows therapists to address issues preemptively, preventing setbacks and optimizing treatment efficacy. Detection of patterns in movement or strength metrics can signal necessary adjustments to therapy plans.
Personalized Therapy Recommendations
AI analyzes comprehensive patient data to generate customized therapy suggestions. These evidence-based recommendations guide therapists in developing optimal exercise regimens, rest periods, and treatment modifications tailored to individual progress and requirements.
Improved Communication and Collaboration
AI-powered platforms facilitate seamless information sharing among patients, therapists, and caregivers. Real-time data access and remote monitoring capabilities enhance coordination, enabling more responsive and effective care delivery.
Objective Assessment and Data-Driven Decisions
AI monitoring systems provide quantifiable progress metrics, reducing reliance on subjective evaluations. These objective insights support more accurate treatment assessments and informed program adjustments based on measurable evidence.
Enhanced Safety and Risk Mitigation
AI contributes to patient safety by detecting potential risks during therapy sessions. Real-time monitoring can identify unsafe movements or excessive strain, triggering alerts to prevent injuries and ensure safe rehabilitation practices.
Future Implications and Ethical Considerations
Long-Term Impact on Rehabilitation Practices
The incorporation of AI into geriatric rehabilitation will fundamentally transform care delivery. Future systems will enable unprecedented personalization of treatment plans, particularly beneficial for patients experiencing age-related cognitive and physical decline. AI's ability to process vast datasets will uncover new insights, leading to more evidence-based and effective rehabilitation protocols.
Ethical Considerations and Data Privacy
As AI adoption increases, protecting patient data becomes critically important. Implementing robust security measures including encryption and access controls is essential. Addressing potential algorithmic bias through rigorous testing and continuous monitoring ensures equitable healthcare delivery across diverse populations.
Accessibility and Equity in Implementation
Ensuring widespread access to AI-powered rehabilitation tools requires addressing technological disparities among both patients and providers. Comprehensive training programs and user-friendly interfaces can help bridge the digital divide while maintaining patient autonomy and dignity in care decisions.