Personalized Medicine through AI-Driven Analysis
Harnessing AI for Precision Diagnostics
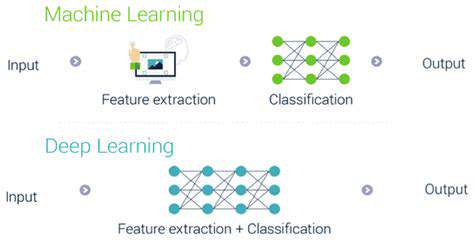
The medical field is witnessing a paradigm shift as artificial intelligence transforms diagnostic capabilities. Modern diagnostic tools powered by machine learning can process extensive patient records, including radiology scans, genomic data, and behavioral patterns, to detect subtle abnormalities that might escape human observation. These advanced systems analyze complex datasets with remarkable precision, facilitating earlier intervention and more accurate treatment pathways. The reduction in diagnostic errors achieved through these technologies represents a major leap forward for healthcare quality assurance.
In radiology departments worldwide, deep learning models demonstrate particular proficiency in interpreting medical imagery. From identifying early-stage tumors in mammograms to detecting minute neurological changes in brain scans, these systems provide clinicians with enhanced diagnostic support. This technological augmentation of human expertise enables more confident clinical decisions and customized patient management plans.
Personalized Treatment Strategies
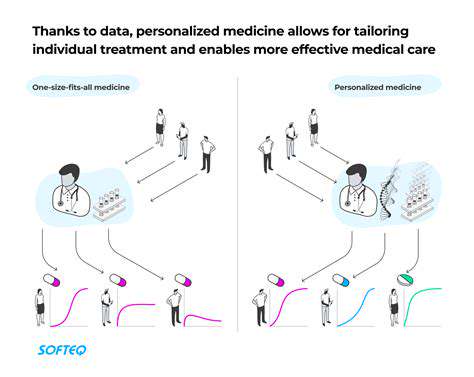
Contemporary medical practice increasingly emphasizes treatment personalization through computational analysis. Sophisticated algorithms evaluate multiple patient-specific factors - including pharmacogenomic profiles, treatment response histories, and environmental influences - to generate optimized therapeutic recommendations. This data-driven approach minimizes the traditional trial-and-error methodology in treatment selection.
In cancer care particularly, molecular profiling of tumors combined with predictive analytics allows oncologists to select chemotherapy regimens with the highest probability of success. Such precision oncology approaches demonstrate how computational medicine can dramatically improve therapeutic outcomes while reducing unnecessary treatment toxicity.
Drug Discovery and Development Acceleration
The pharmaceutical industry benefits tremendously from artificial intelligence applications throughout the drug development pipeline. Machine learning models screen millions of molecular compounds against biological targets, identifying potential drug candidates with optimal binding characteristics and safety profiles. This computational approach significantly compresses the traditional drug discovery timeline, potentially bringing life-saving medications to patients years earlier.
Predictive modeling also revolutionizes clinical trial design by forecasting probable outcomes based on preclinical data. These simulations enable more efficient resource allocation, focusing research efforts on the most promising therapeutic candidates while reducing financial risks associated with failed trials.
Improving Patient Outcomes
The ultimate goal of computational medicine manifests in enhanced clinical results across healthcare systems. By enabling precisely targeted interventions tailored to individual patient characteristics, these technologies reduce treatment durations, minimize adverse effects, and improve quality-adjusted life years. This shift toward personalized preventative care represents a fundamental transformation in healthcare delivery models worldwide.
Predictive analytics also empower proactive health management by identifying at-risk individuals before symptom onset. Such anticipatory medicine approaches could potentially prevent many chronic conditions through early lifestyle interventions or preemptive treatment.
Genetic Data Integration
Modern therapeutic strategies increasingly incorporate comprehensive genomic analysis to guide clinical decision-making. Advanced bioinformatics tools process complex genetic information to identify disease predispositions and predict medication responses, enabling truly personalized prevention and treatment regimens based on each patient's unique DNA profile.
Ethical Considerations in AI-Driven Healthcare
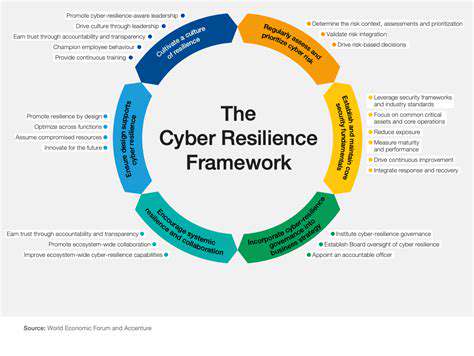
As computational technologies permeate medical practice, several ethical imperatives demand attention. Protecting sensitive health data requires robust cybersecurity measures and transparent data governance policies. Algorithmic fairness must be rigorously evaluated to prevent bias in diagnostic or treatment recommendations. Thoughtful regulatory frameworks that balance innovation with patient safety remain essential for responsible technology adoption in healthcare.
Equity concerns also emerge regarding access to these advanced technologies. Ensuring broad availability of computational medicine tools across diverse socioeconomic groups and geographic regions represents an ongoing challenge for healthcare systems worldwide.
Accessibility and Affordability of Care
Automation and efficiency gains from computational medicine could potentially reduce healthcare costs while expanding service availability. By streamlining diagnostic workflows and optimizing treatment selection, these technologies may help make high-quality care more economically accessible. The economic implications of widespread AI adoption could fundamentally reshape healthcare financing models and improve population health metrics.
Operational efficiencies achieved through predictive analytics and automated decision support may enable healthcare providers to serve larger patient populations without compromising care quality - a critical factor in addressing global healthcare disparities.
Future Directions and Challenges
Future Directions in AI-Powered Biomedical Signal Processing
The evolution of biomedical signal analysis technologies continues to accelerate, with several promising research trajectories emerging. Next-generation algorithms demonstrate improved capacity to handle the natural variability in physiological measurements, incorporating advanced noise reduction techniques and adaptive learning architectures. These developments enable more reliable interpretation of complex biosignals across diverse patient populations and clinical scenarios.
Integration of multimodal data streams represents another exciting frontier. Combining continuous monitoring from wearable devices with traditional diagnostic imaging creates comprehensive patient health profiles, enabling earlier detection of pathological changes. Concurrently, the field prioritizes developing interpretable machine learning models that provide clinically meaningful explanations for their analytical outputs, fostering greater trust among medical professionals.
Challenges in Implementing AI for Biomedical Signal Processing
Despite remarkable progress, significant implementation barriers persist. Curating sufficiently large and representative training datasets remains resource-intensive, requiring extensive multicenter collaborations while maintaining strict data privacy standards. Validation protocols must ensure consistent performance across diverse clinical environments and patient demographics before widespread deployment.
Integration challenges extend to healthcare infrastructure, where existing systems often lack compatibility with advanced analytical tools. Comprehensive staff training programs and workflow redesign become necessary to realize the full potential of these technologies in clinical practice. Perhaps most critically, ongoing vigilance is required to identify and mitigate potential biases in algorithmic decision-making that could disproportionately affect specific patient groups.
Regulatory agencies continue developing appropriate oversight frameworks that encourage innovation while ensuring patient safety. These evolving standards must address unique aspects of machine learning systems, including their dynamic learning capabilities and potential for unexpected behavior patterns.