Introduction to AI-Augmented Clinical Processes
Understanding the Core Concept
AI-augmented clinical practices represent a transformative evolution in modern healthcare, where artificial intelligence technologies work alongside medical professionals to enhance clinical decision-making. Rather than replacing human expertise, these tools provide supplementary insights that enable healthcare providers to deliver more precise and timely care. At its heart, this approach seeks to bridge the gap between data overload and clinical actionability by surfacing relevant patterns in patient data. The synergy between clinician intuition and machine analysis creates a powerful dynamic for improving both individual patient outcomes and systemic healthcare efficiency.
Applications in Diagnostics
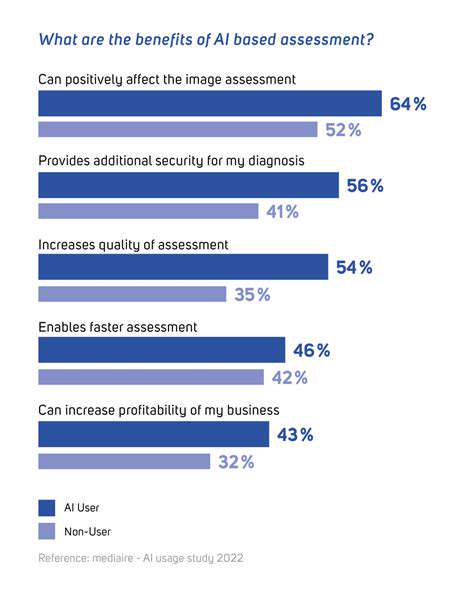
In diagnostic medicine, AI demonstrates particular promise for imaging interpretation. Advanced pattern recognition algorithms can process radiographic studies with both speed and nuance, detecting subtle tissue changes that might escape initial human observation. This capability proves especially valuable in time-sensitive situations where early detection dramatically impacts treatment success rates.
What makes these systems particularly valuable is their ability to contextualize findings within broader patient histories, comparing current imaging against previous studies and population-level data to identify clinically significant changes. This comprehensive analysis supports radiologists in making more confident diagnostic determinations while reducing interpretation variability.
Improving Treatment Efficacy
Therapeutic decision-making benefits significantly from AI's ability to synthesize complex patient variables. By integrating clinical history, genomic data, treatment responses from similar cases, and emerging research findings, these systems can suggest tailored intervention strategies. Perhaps most importantly, AI models can predict individual patient responses to specific therapies, helping clinicians avoid ineffective treatments and unnecessary side effects. This precision approach represents a major advance beyond the traditional one-size-fits-all treatment paradigm.
Enhancing Administrative Efficiency
Healthcare systems increasingly deploy AI to streamline operational workflows that traditionally consumed substantial staff time and resources. Intelligent automation handles routine tasks like appointment coordination, documentation, and insurance processing with consistent accuracy. This operational transformation allows clinical staff to redirect their energy toward direct patient care while simultaneously reducing administrative overhead costs. The resulting efficiency gains help healthcare organizations manage growing patient volumes without compromising service quality.
Ethical Considerations and Future Directions
As AI integration deepens, maintaining appropriate oversight remains crucial. Key concerns include ensuring algorithm transparency, protecting sensitive health data, and preserving the essential human elements of medical practice. Moving forward, the most effective implementations will likely combine AI's analytical strengths with clinicians' experiential wisdom, creating collaborative systems that enhance rather than replace human judgment. Ongoing multidisciplinary dialogue will be essential to navigate these complex implementation challenges responsibly.
AI's Role in Diagnostic Accuracy and Speed
AI's Impact on Diagnostic Speed
The temporal advantages of AI in medical imaging analysis cannot be overstated. Modern diagnostic algorithms can process complex imaging studies in fractions of the time required for human interpretation, a capability that proves particularly vital in emergency situations. This rapid processing translates directly to faster treatment initiation, often making the difference between positive and negative clinical outcomes. Emergency departments leveraging this technology report significantly reduced door-to-treatment times for stroke and trauma cases.
Beyond emergency applications, this processing speed also alleviates diagnostic backlogs in routine care settings, ensuring patients receive timely answers without unnecessary anxiety. The ability to prioritize cases based on algorithmic risk assessment further optimizes radiologist workflow and resource allocation.
Enhanced Diagnostic Accuracy Through Pattern Recognition
AI systems derive their diagnostic power from exposure to vast annotated image libraries, developing recognition capabilities that exceed human visual perception thresholds. These systems detect subtle density variations, textural changes, and spatial relationships that might escape even experienced radiologists during prolonged reading sessions. In mammography, for instance, AI tools consistently identify microcalcifications and architectural distortions associated with early-stage breast cancer that human readers might overlook.
The continuous learning nature of these systems means their accuracy improves over time as they process more cases. This contrasts with human practitioners, whose pattern recognition skills plateau after accumulating certain experience levels.
Minimizing Human Error in Diagnostics
Diagnostic medicine inevitably suffers from human factors like fatigue, distraction, and cognitive biases. AI systems provide an objective second read that remains consistent regardless of caseload volume or time of day. By handling initial image screening and flagging potential abnormalities, these tools reduce diagnostic oversights while allowing radiologists to concentrate their expertise on complex cases requiring nuanced interpretation.
This collaborative model enhances overall diagnostic quality while maintaining appropriate physician oversight. The result is a healthcare system that leverages the respective strengths of human and artificial intelligence.
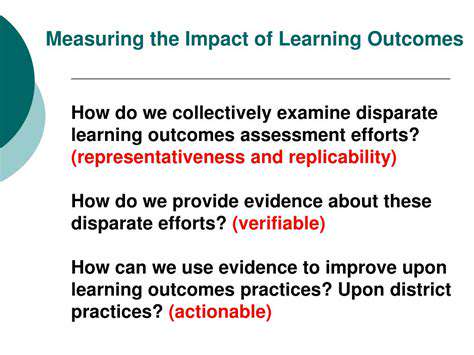
The Role of Data in AI's Diagnostic Capabilities
AI diagnostic performance directly correlates with training data quality and diversity. Comprehensive datasets representing various demographics, disease stages, and imaging modalities enable algorithms to develop robust recognition capabilities across diverse patient populations. Ongoing data collection and annotation efforts remain critical for improving algorithm generalizability and reducing diagnostic blind spots.
Emerging federated learning approaches allow algorithms to learn from distributed datasets while maintaining patient privacy, potentially overcoming one of the major barriers to comprehensive medical AI training.
Challenges and Future Directions
Successful AI integration requires addressing several implementation challenges. Algorithm explainability remains crucial for clinician trust and adoption, as practitioners need to understand the basis for AI-generated findings. Regulatory frameworks must evolve to ensure patient safety without stifling innovation. The most promising path forward involves developing hybrid diagnostic systems that combine AI's processing power with human clinical judgment for optimal patient care.
Continued progress will depend on sustained collaboration between technologists, clinicians, and policymakers to create standards that maximize benefits while mitigating risks.
Streamlining Administrative Tasks with AI
Automating Data Entry
Intelligent data capture systems transform unstructured clinical notes into organized, actionable information within electronic health records. These solutions employ natural language processing to extract relevant clinical concepts from physician dictations and other free-text sources, dramatically reducing manual data entry burdens. The resulting structured data facilitates more accurate billing, quality reporting, and clinical decision support.
Intelligent Scheduling and Resource Allocation
Advanced scheduling algorithms analyze numerous variables - including provider availability, patient needs, equipment requirements, and historical patterns - to optimize clinic flow. These systems dynamically adjust schedules in response to cancellations or emergencies, maximizing resource utilization. Some implementations have reduced patient wait times by over 30% while simultaneously increasing provider productivity through better time management.
Improved Communication and Collaboration
AI-enhanced communication platforms analyze clinical documentation to identify care coordination needs automatically. These systems can prompt necessary consultations, flag medication reconciliation requirements, and ensure appropriate follow-up planning. By surfacing these coordination requirements proactively, the technology reduces communication gaps that traditionally contributed to medical errors and care delays.
Enhanced Patient Intake and Triage
Smart intake systems streamline registration by auto-populating forms from existing records and verifying insurance eligibility in real-time. AI-driven symptom checkers and virtual triage tools help prioritize patients based on clinical urgency, ensuring those needing immediate attention receive it promptly. These innovations have proven particularly valuable in emergency departments and urgent care settings where rapid patient assessment is critical.
Predictive Analytics for Resource Management
By analyzing historical admission patterns, seasonal illness trends, and community health indicators, AI tools forecast patient volumes with remarkable accuracy. Hospital administrators use these predictions to adjust staffing levels, bed allocations, and supply inventories proactively. This forward-looking approach prevents both resource shortages during peak demand and wasteful overstaffing during slower periods.
Proactive Identification of Potential Issues
Continuous analysis of clinical and operational data allows AI systems to identify emerging risks before they escalate. These might include potential medication interactions, early signs of hospital-acquired infections, or administrative bottlenecks in care delivery. Early warning systems enable preventative interventions that maintain care quality while avoiding costly complications.
Automated Reporting and Compliance
Regulatory reporting represents a significant administrative burden for healthcare organizations. AI solutions automate quality measure calculation, adverse event documentation, and other compliance requirements. This automation ensures consistent, auditable reporting while freeing clinical staff to focus on patient care rather than paperwork.